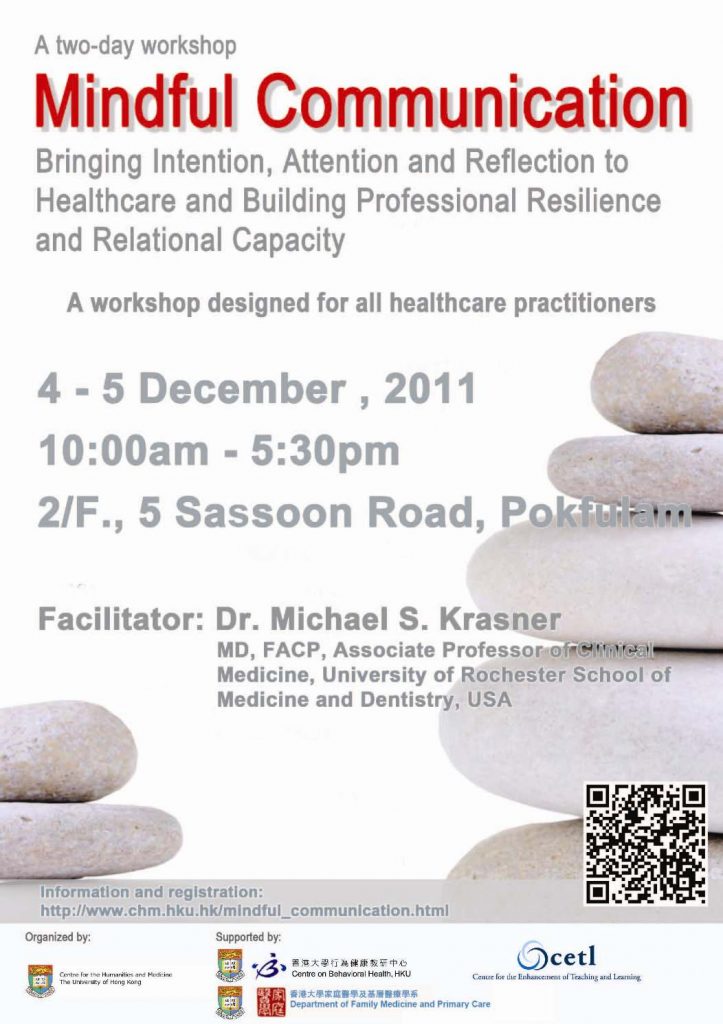
Date: 4 – 5 December 2011
Time: 10:00am – 5:30pm
Venue: 2/F., The Hong Kong Jockey Club Building for Interdisciplinary Research, 5 Sassoon Road, Pokfulam
Overview
In response to the increasing pace and complexity of medical practice, physicians and other health professionals are experiencing unprecedented levels of job dissatisfaction and burnout, affecting their sense of well-being and the quality of care they provide. A powerful but under recognized approach to these challenges is to enhance the practitioners’ capacity for mindfulness.
Mindfulness in medicine refers to the ability to be aware, in the present moment, on purpose, with the intention of providing better care to patients and of taking better care of oneself. Mindfulness is at the core of clinical competence, and includes the capacities for critical curiosity, attentive observation, beginner’s mind, and presence. The proposed program will give participants the skills and tools necessary to bring mindful communications into daily clinical practice and continuing education.
Research suggests that courses in mindful practice and mindful communication can result in lower burnout and greater well-being, empathy and patient-centered care. In addition, mindful practice may result in fewer errors, a greater sense of presence, the ability to see a situation from multiple perspectives before reacting, and greater satisfaction from work. Our current health care environment makes mindful practice very challenging.
Accordingly, this workshop will address these external barriers as well as participants’ and learners own internal barriers to self-awareness such as unexamined emotions, premature closure, over concreteness and emotional exhaustion – which then manifest as feeling overwhelmed by suffering, ignoring the obvious, treating others like objects, withdrawing from unpleasant or anxiety-provoking situations, having difficulty tolerating ambiguity and uncertainty, and making hasty decisions.
Learning Objectives
– Describe the problem of healthcare professionals burnout and its implications for health care delivery
– Describe the effects of mindfulness-based interventions on physician well-being and relational capacity
– Illustrate the application of narrative medicine and appreciative dialogue in the setting of contemplative and medical practice
– Discuss ways in which this approach may be applicable to the work environment
Intended Audience
All healthcare practitioners, including physicians, medical school faculty, nurses, social workers, and therapists, are welcome.
Workshop Outline
DAY 1 (4 December 2011)
This first day will be devoted to establishing an experiential understanding of mindfulness meditation, narrative medicine, and the application of appreciative inquiry in interpersonal dialogue. Participants will work together in large and small groups, with didactic elements built into the experiential exercises. The practice will center on themes of 1) the Present Moment; 2) Perception and Surprise; and 3) Teamwork. Participants are encouraged to use clinical experience as the source material for the narrative development and appreciative dialogues.
| 9:30 AM to 10:00 AM | Registration |
| 10:00 AM to 12:30 PM | Introductions Mindfulness Practices What is Narrative Medicine and Appreciative Inquiry? The Present Moment: Narrative and Appreciative Dialogue |
| 12:30 PM to 1:30 PM | Light Lunch |
| 1:30 PM to 5:30 PM | Mindfulness Practice Perception and Surprise Narrative and Appreciative Dialogues Teamwork Review, debrief, and wrap-up |
DAY 2 (5 December 2011)
This second day will be devoted to deepening the meditative practice and working with challenging clinical themes in the development of narratives and the sharing in appreciative dialogues. These themes include 1) Stressful Communication; 2) Health Professional Burnout; and 3) Mindful Practice and its Relationship to the Suffering Dimension in Clinical Practice. As the practice of mindfulness deepens, participants will bring a greater degree of nonjudgmental moment-to-moment awareness to their reflections relating to these themes, and will begin to experience the presence of meditative awareness in the midst of interpersonal dialogue. A final period will be devoted to exploring the personal, clinical, and other professional applications of Mindful Communication.
| 10:00 AM to 12:30 PM | Mindfulness Practices Stressful Communication Discussion, Narrative and Appreciative Dialogue |
| 12:30 PM to 1:30 PM | Light Lunch |
| 1:30 PM to 5:30 PM | Mindfulness Practices Health Professional Burnout Discussion, Narrative and Appreciative Dialogues Mindful Practice and its Relationship to the Suffering Dimension in Clinical Practice Discussion, Narrative and Appreciative Dialogues Mindful Communication Applications |
Programme Fees
| On or before 15 October, 2011 (early bird rate) | HK$1250 |
| After 15 October, 2011 | HK$1500 |
Deadline for registration and payment: 15 November, 2011
*The programme fees include all course materials, lunch and snacks for two days, facilities and venue. All programme fees are non-refundable.
We accept cheques only. Once you have registered, a registration number will be assigned to you. An email will also be sent to you to acknowledge the receipt of the registration. Please send your cheque (with your name and registration number on the back), payable to The University of Hong Kong, to:
Centre for the Humanities and Medicine, The University of Hong Kong,
Room 148, Main Building, Pokfulam Road.
An email confirmation will be sent to you once we have received your cheque.
*Payment must be settled within two weeks after you have completed the registration.
* Participants are strongly recommended to dress comfortably and bring a towel or mat to lie on.
Deadline for registration and payment: 15 November, 2011
Enquiries: chm1@hku.hk or (852) 2859 2867.
CHM Accreditation
CME Programme for practising doctors who are not taking CME programme for specialists – 7 points each for Day1 and 2
| Organization | Points awarded | ||
| Dec 4 | Dec 5 | Whole Function | |
| Hong Kong College of Anaesthesiologists | Nil | Nil | Nil |
| Hong Kong College of Community Medicine | 6 | 6 | 10 |
| College of Dental Surgeons of Hong Kong | 6.5 (Cat. B) | 6.5(Cat. B) | 13(Cat. B) |
| Hong Kong College of Emergency Medicine | Nil | Nil | Nil |
| Hong Kong College of Family Physicians | 5 (Cat. 5.2) | 5 (Cat. 5.2) | 10 (Cat. 5.2) |
| Hong Kong College of Obstetricians & Gynaecologists | 5(Non O&G) | 5 (Non O&G) | 10(Non O&G) |
| College of Ophthalmologists of Hong Kong | 3 (passive) | 3 (passive) | 4 (passive) |
| Hong Kong College of Orthopaedic Surgeons | 5 (Cat. B) | 5 (Cat. B) | 10(Cat. B) |
| Hong Kong College of Otorhinolaryngologists | 3.5 | 3.5 | 7 (Cat. 2.2) |
| Hong Kong College of Paediatricians | 6 (Cat. E) | 6 (Cat. E) | 10 (Cat. E) |
| Hong Kong College of Pathologists | 3 (passive) | 3 (passive) | 6 (passive) |
| Hong Kong College of Physicians | 6 | 6 | 12 |
| Hong Kong College of Psychiatrists | 5 (OT/IP) | 5 (OT/IP) | 10 (OT/IP) |
| Hong Kong College of Radiologists | 4 (Cat. B) | 4 (Cat. B) | 8 (Cat. B) |
| The College of Surgeons of Hong Kong | 6 (passive) | 6 (passive) | 12(passive) |
| MCHK CME Programme | – | – | – |
Organized by:
Centre for the Humanities and Medicine, HKU
Presented by:
Centre for the Enhancement of Teaching and Learning, HKU
Centre on Behavioral Health, HKU
Department of Family Medicine and Primary Care, HKU
